CBCT Changing the Practice of Oral and Maxillofacial Surgery
Gary Orentlicher, DMD | Andrew Horowitz, DMD, MD | Batya Goldwaser, DMD, MD
The past decade has seen dental and surgical diagnosis and planning rapidly shift from 2-dimensional (2D) methods to 3-dimensional (3D). Few innovations have impacted the practice of dentistry and oral and maxillofacial surgery as dramatically as cone-beam computed tomography (CBCT) digital technologies. These low-radiation, highly accurate, small-footprint machines have transformed the way clinicians practice daily. Combined with intraoral and model-based optical scanners, 3D printing and stereolithographic technologies, and proprietary software applications that are designed to move these technologies from theory to practice, dentistry and surgery are undergoing a digital transformation.
CBCT and digital technologies have become embedded in the authors’ oral and maxillofacial surgery practice in many ways. Some key examples are discussed in the following paragraphs.
Dentoalveolar Surgery
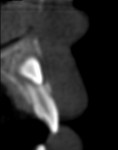
In some situations, determining the location of impacted and supernumerary teeth for the purpose of extraction or surgical exposure can be very difficult. When using 2D periapical and panoramic radiographs alone, it may not be possible to gauge the proximity, angulations, and locations of these teeth relative to surrounding vital structures, adjacent teeth, and/or implants1 (Figure 1 through Figure 3).
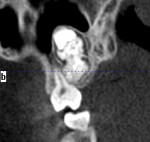
Similarly, the relationship between impacted third molars and the mandibular nerve canal is difficult to assess using conventional 2D radiographic techniques.2-4 The buccal-lingual position of the mandibular canal has not been found to be consistently more buccal or lingual; therefore, the clinician often functions on a “best guess” based on panoramic radiographic signs.5 With an overall incidence of inferior alveolar nerve injury secondary to third molar removal of 0.5% to 8%6-8 but a less than 1% incidence of permanent numbness,8-10 being able to preoperatively determine those cases at highest risk with a 3D CT/CBCT can be invaluable.11
Preprosthetic and Dental Implant Surgery
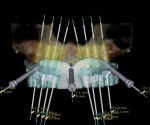
From simple implant site evaluation to full-arch implant reconstruction, CBCT has revolutionized the practice of dental implantology. Three-dimensional–guided surgery techniques and instrumentation have greatly increased the accuracy of implant placement and enabled a multidisciplinary team approach that is restoratively driven. The result is improved patient treatment satisfaction and outcomes.
In implant sites of questionable bone contour or volume, a preoperative CT/CBCT scan aids in determining the need for and the type of bone grafting. Fabricating a scanning appliance for the patient to wear during the scan, and then importing the data into proprietary implant planning software applications, allows the visualization of bone in the planned implant site(s) in relation to the ideal position of the planned restoration(s).12 “Virtual” placement of implants in these images can provide information regarding the location and volume of bone in planned sites. Measurement and bone volume tools can be used for preoperative planning of appropriate graft procedures for site and graft dimensions and volume (ie, block bone, ridge splitting, particulate bone, sinus lift, or distraction osteogenesis).
In the maxilla, anatomic variations such as the lateral maxillary wall thickness, proximity of the maxillary buttress, and size and location of bony septae within the sinus can be determined prior to “sinus lift” graft procedures. Intraoral block bone graft donor sites (ie, chin, external oblique ridge, tuberosity) can be evaluated for bone thickness and proximity to nerves and root apices. Measurements of these relationships can be used to harvest donor bone grafts with less potential patient morbidity.
Maxillofacial Trauma
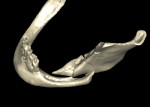
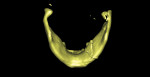
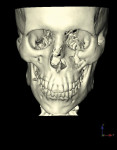
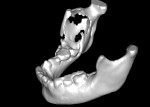
CT/CBCT data from maxillofacial trauma patients can provide 3D reformatted images that give the trauma surgeon a unique perspective of the nature of the injury and the degree of displacement of the fracture segments, which helps guide the appropriate surgical approaches for the fracture reduction and stabilization13 (Figure 4 through Figure 6). Stereolithographic models can also be made that provide the surgeon with 3D models that can be used for further diagnosis and creation of custom implants and/or plates. In delayed trauma reconstruction, it can be difficult to create symmetry with the uninjured side, making custom plates invaluable.14
Pathology and Reconstruction
The treatment of pathologic lesions of the mouth and jaws can present difficult surgical and reconstructive dilemmas. Frequently these problems require extensive removal of diseased and healthy tissue and bone, leaving small and large functional and esthetic defects. Despite preoperative education, patients are often surprised at the extent of the surgical procedures needed and the resultant functional and esthetic defects.
Analysis of preoperative CT/CBCT scan axial, coronal, sagittal, cross-sectional, and panoramic views in 0.5-mm to 1-mm–thick cuts, along with 3D reconstructions, can be instrumental in localizing lesions, measuring the extent of the pathology, and determining involvement of surrounding vital structures and teeth (Figure 7 and Figure 8). These images can also be used postoperatively to measure the contours of the resulting deformity to determine the volume of potential bone grafts for reconstruction. One-to-one stereolithographic models can be used to plan surgical resection margins, pre-bend reconstruction plates, and plan bone grafts (Figure 9). This can reduce operative time, minimize surgical trauma and patient morbidity, and maximize functional and esthetic outcomes.13
Orthognathic and Craniofacial Surgery
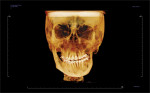
CT/CBCT scans with 3D imaging are a routine tool used to diagnose and treatment plan dentofacial patients undergoing orthognathic surgery. With the help of specialized software, the surgeon can “virtually” plan complex movements of the maxilla, mandible, and/or chin in 3D. Three-dimensional printing technologies are used to create stabilization appliances and, in some cases, highly accurate cutting guides. Additionally, the predictable localization and measurement of vital anatomic structures in the maxilla and mandible preoperatively may translate into shortened procedure time and minimize potential surgical risks and complications.15
By inserting patient soft- and hard-tissue information into various software applications, statistical population norms can be used for customized facial implant fabrication. These implants are manufactured from biocompatible materials to a patient’s specific bony anatomy. Custom facial implants can be created for any area of the facial skeleton (ie, chin, malar, mandibular angle, and infraorbital regions).16
Summary
A dentist or surgeon’s goal is to maximize the amount of preoperative information to facilitate successful outcomes while minimizing trauma and potential risks to the patient. As with any new technology, practitioners must use their knowledge—and creativity—to recognize its applicability in generating solutions for dental, surgical, and reconstructive dilemmas. Successful integration in practice requires a commitment of both time and finances to learn how to use the tools and move beyond natural fears of potential failure.
References
1. Walker L, Enciso R, Mah J. Three-dimensional localization of maxillary canines with cone-beam computed tomography. Am J Orthod Dentofac Orthop. 2005;128(4):418-423.
2. Friedland B, Donoff B, Dodson TB. The use of 3-dimensional reconstructions to evaluate the anatomic relationship of the mandibular canal and impacted mandibular third molars. J Oral Maxillofac Surg. 2008;66(8):1678-1685.
3. Klinge B, Petersson A, Maly P. Location of the mandibular canal: comparison of macroscopic findings, conventional radiography, and computed tomography. Int J Oral Maxillofac Implants. 1989;4(4):327-332.
4. Koong B, Pharoah MJ, Bulsara M, Tennant M. Methods of determining the relationship of the mandibular canal and third molars: a survey of Australian oral and maxillofacial surgeons. Aust Dent J. 2006;51(1):64-68.
5. Ohman A, Kivijärvi K, Blombäck U, Flygare L. Pre-operative radiographic evaluation of lower third molars with computed tomography. Dentomaxillofac Radiol. 2006;35(1):30-35.
6. Rood JP. Permanent damage to inferior alveolar and lingual nerves during the removal of impacted mandibular third molars. Comparison of two methods of bone removal. Br Dent J. 1992;172(3):108-110.
7. Sisk AL, Hammer WB, Shelton DW, Joy ED Jr. Complications following removal of impacted third molars: the role of the experience of the surgeon. J Oral Maxillofac Surg. 1986;44(11):855-859.
8. Bruce RA, Frederickson GC, Small GS. Age of patients and morbidity associated with mandibular third molar surgery. J Am Dent Assoc. 1980;101(2):240-245.
9. Alling CC. Dysesthesia of the lingual and inferior alveolar nerves following third molar surgery. J Oral Maxillofac Surg. 1986;44(6):454-457.
10. Wofford DT, Miller RI. Prospective study of dyesthesia following odontectomy of impacted mandibular third molars. J Oral Maxillofac Surg. 1987;45(1):15-19.
11. Maegawa H, Sano K, Kitagawa Y, et al. Preoperative assessment of the relationship between the mandibular third molar and the mandibular canal by axial computed tomography with coronal and sagittal reconstruction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2003;96(5):639-646.
12. Orentlicher G, Goldsmith D, Abboud M. Computer-guided planning and placement of dental implants. Atlas Oral Maxillofac Surg Clin North Am. 2012;20(1):53-79.
13. Orentlicher G, Goldsmith D, Horowitz A. Applications of 3-dimensional virtual computerized tomography technology in oral and maxillofacial surgery: current therapy. J Oral Maxillofac Surg. 2010;68(8):1933-1959.
14. He D, Zhang Y, Ellis E. Panfacial fractures: analysis of 33 cases treated late. J Oral Maxillofac Surg. 2007;65(12):2459-2465.
15. Gelesko S, Markiewicz MR, Weimer K, Bell RB. Computer-aided orthognathic surgery. Atlas Oral Maxillofac Surg Clin North Am. 2012;20(1):107-118.
16. Goldsmith D, Horowitz A, Orentlicher G. Facial skeletal augmentation using custom facial implants. Atlas Oral Maxillofac Surg Clin North Am. 2012;20(1): 119-134.
About the Authors
Gary Orentlicher, DMD
Section Chief, Division of Oral and Maxillofacial Surgery
White Plains Hospital
White Plains, New York
Private Practice
New York Oral, Maxillofacial, and Implant Surgery
Scarsdale, New York
Andrew Horowitz, DMD, MD
Associate Attending, White Plains Hospital
White Plains, New York
Private Practice
New York Oral, Maxillofacial, and Implant Surgery
Scarsdale, New York
Batya Goldwaser, DMD, MD
Attending Oral and Maxillofacial Surgeon
White Plains Hospital
White Plains, New York
Private Practice
New York Oral, Maxillofacial, and Implant Surgery
Scarsdale, New York
CBCT Case Integration
The introduction of CT/CBCT and digital technologies has changed the way the authors practice oral and maxillofacial surgery. Integrating these technologies into daily practice has improved diagnosis, planning, and patient outcomes. The following pictorial illustrations represent the ways that CBCT can be incorporated for success in preprosthetic and dental implant surgery (Figure 10 through Figure 16); and orthognathic and craniofacial surgery (Figure 17 through Figure 22).