The Esthetic Solution to Immediate Complete Removable Prosthetics
Treatment plan for functional and esthetic prosthesis
Eugene Royzengurt, DTG
In the world of removable prosthetics, dental technicians are constantly challenged by difficult treatment plans and sometimes find it nearly impossible to find a feasible solution to a complex issue. A large portion of treatment planning is based on more than just the clinician’s knowledge and understanding of the situation; typically, the patient dictates it. Immediate dentures are a prime example.
As many technicians know, immediate prosthodontics are not as desirable in definitive treatment planning as the properly fabricated complete denture for a fully edentulous arch.1 However, because of the significant price difference, patients often opt out of receiving the secondary complete prosthetic and utilize an immediate denture simply as a temporary transitional appliance. The option of extracting the entire dentition and allowing a proper healing period before fabricating a definitive complete removable prosthesis is also not an option in many situations due to patients’ concerns for esthetics. Considering these parameters, an immediate complete removable prosthetic typically is the definitive option for the restoration. Furthermore, this will be the patient’s first complete removable restoration and often will set the standard in the patient’s mind for restorative treatment that follows. Because this is often the case, technicians must attempt to create the most functional and esthetic prosthesis as possible.
Case Report
A 62-year-old female presented with terminal upper and lower dentition and was given a treatment plan for full-mouth extractions and complete upper and lower removable dentures (Figure 1). Due to the patient’s esthetic and monetary concerns, the treatment plan called for immediate complete prosthetics. Most of the dentition was primarily in the anterior, and a decision was made to not extract any posterior teeth until the day of the delivery.
At the initial appointment, preliminary maxillary and mandibular impressions were taken with stock trays and alginate impression material. The impressions were immediately poured up in Type III model stone (Hi-Tec Dental, hi-tecdental.com) to reduce any type of distortion and then sent to the laboratory for the fabrication of custom trays. Once the casts were trimmed and evaluated for defects, the models were blocked out with a single sheet of baseplate wax in the edentulous areas, with 2 sheets of baseplate wax placed in the dentate regions. Tissue stops were placed in the proper anatomic areas. (Note: It helps if the clinician evaluates the tissue and relays that information to the technician so the tissue stops are placed properly.) Custom trays were fabricated using the viable light cure material (Megatray, Select Dental Manufacturing, selectdentalmfg.com) with the handle placed in the proper position to avoid hindering the movement of facial muscles and allow for a fully functional impression. The borders were trimmed 2 mm to 3 mm short of the vestibule in order to allow for the border molding to be accomplished.2
During the second appointment, the clinician checked the custom trays and trimmed the muscle area in order to allow a full range of muscle movement at the impression stage. This step is particularly important with lower dentures. This region has high myodynamics and, if not properly impressed, the prosthesis fit will not be stable. The impression was border molded with heavy-body vinyl polysiloxane (VPS) (Splash, Den-Mat Holdings, denmat.com). Regular-viscosity VPS impression material was used for the body of the impression. Wash impression material was not used in this case, though it is often used for this procedure. At this point, the impressions were sent to the laboratory to fabricate wax rims for vertical adjustments and bite registration.
When the laboratory received the final impressions, they were allowed to sit for at least 12 hours from the time of pickup from the dentist. This allowed the gases to escape from the VPS material, which would otherwise distort the master cast by introducing small bubbles into it. The final impression was then boxed and beaded using Wonderfill (Dental Creations, wonderfill.com) material and magnetic boxing strips. The depth was checked in order to allow at least 15 mm at the lowest portion of the master cast.3 The impression was sprayed with surfactant in order to minimize bubbles. The Type III model stone was vacuum mixed and poured slowly in order to produce a precise master cast. Once the stone was fully set, it was separated and trimmed to produce a land area on the cast of 4 mm to 5 mm around. Because the clinician determined that the patient’s vertical dimensions would remain the same and the existing occlusal stops were present, the bite rims would simply be used to stabilize the models and would not be utilized in any changes of vertical dimension. The maxillary bite plane was followed in this case from the edge of the upper incisors to the hamular notches and the mandibular bite rim from the edge of the lower incisors to three-quarters of the retromolar pads.
Then, the clinician recorded the bite, in this case using a stick bite record (Figure 2). The clinician also recorded the gingival shade in order to match the wax-up as closely as possible to the final prosthesis (Figure 3). The tooth shade and any mold changes were recorded and given to the laboratory. Changes in position of the anterior teeth were also addressed at this time. Clinical photography was provided to further assist the technician in fabricating the final prosthesis.
The laboratory received the case and preserved the bite record by attaching metal pins onto the casts with the help of a hot-glue gun, which allows for greater precision compared with using rubber bands. The case was mounted on the Stratos 200 articulator (Ivoclar Vivadent, ivoclarvivadent.com) with the upper incisors in line with the guide notch on the incisor pin and the retromolar pads in line with the notch on the posterior supports of the articulator. The casts were placed parallel to the articulator with the help of the stick bite (Figure 4). All the steps had to be approximated because the facebow or a facial analyzer system was not used. The mountings were allowed to set and then were trimmed and polished with sandpaper (Figure 5).
Upon evaluation of the mounted casts, it was clearly visible that the existing dentition was canted to the left, and the photographs further supported this determination. The plane of occlusion needed to be changed at this point, using the tripod occlusion determination method. After collaboration with the clinician as well as several technician colleagues, the technician decided to use tooth No. 8 as the anterior point of the tripod and the line drawn from the incisal edge of tooth No. 8 to the three-quarter mark of the retromolar pad as the plane of occlusion. All the dentition, except for tooth No. 8, was removed from the maxillary and mandibular casts. An additional 1 mm was removed from the cast around the free gingival region in order to compensate for the tissue sinking during the extraction. Using laboratory putty and the aluminum bite plane, a new plane of occlusion was established (Figure 6).
At this point, the modified model analysis was performed.4 On the maxillary, the midline was marked and the tuberosities were outlined. The fovea palatine and palatine raphe were also marked, and the posterior palatal seal was carved arbitrarily. The peripheral vestibule was marked in order to show the final outline of the denture as well as the buccal limit placement of the posterior maxillary dentition. The incisive papilla and the crest of the ridge were also marked. On the mandible, the retromolar pad was outlined and the three-quarter mark was placed. The midline was transferred onto the cast, and the vestibule was marked to show the final outline of the denture. The crest of the ridge was marked, and a line was drawn from the retromolar pad to the area of the first premolar to show the middle of the posterior ridge. A modified compass was used to mark the lowest point of the mandibular ridge. The rise of the mandibular ridge after the lowest point was also marked.
The type of occlusion was selected with the help of the clinician. For this case, the dentist chose lingualized occlusion. The ridge allowed for such an occlusal scheme, and the need for a long and wide centric was met.5 The tooth mold and shade were chosen according to the clinician’s prescription.
With tooth No. 8 still in place, teeth Nos. 9, 10, and 11 were waxed into place and verified (Figure 7). Tooth No. 8 was removed from the cast and replaced by an acrylic tooth along with teeth Nos. 6 and 7. Lower anterior teeth were placed with a 1-mm overbite and 1-mm overjet. The largest lower molar was placed at the lowest point of the mandibular ridge. The model analysis also showed that this would be the last masticatory unit of the mandible, so a compensating curve of 15° was introduced in the tooth placement. The lower premolars were then placed bilaterally. The maxillary posteriors were set and the case was balanced, allowing only for the upper posterior lingual cusps and the lower central fossa to be in centric occlusion. This patient had lingualized occlusion in which the maxillary buccal cusps are not in function and the mandibular buccal cusps are used for balancing. The lingual cusps and central fossa of the mandibular posteriors are used for function. A slight sliding occlusion in protrusive and excursive movements between the maxillary and the mandibular anteriors could be observed.
Because the wax-up could not be removed from the master cast, some guesswork was necessary in waxing to final contour. Using an endodontic file with a rubber stopper helped verify the wax thickness in critical regions. The putty impression was taken of the rugae region in order to transfer those contours into the wax-up. Using photographs and the gingival shade provided, a similar color of wax blends was used to create a more natural appearance.
The final wax-up was cleaned and polished with the use of a soft Abbott Robinson brush and a circular piece of foam mounted on the mandril, respectively. Several photographs of the wax-up were sent to the clinician and patient for evaluation (Figure 8).
During the evaluation of the final wax-up, the decision was made to recreate the palatal anatomy in order to stabilize the denture during swallowing. This was accomplished with the use of a putty matrix impression from the master cast, and it was transferred onto the wax-up (Figure 9).
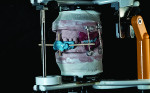
With clinician and patient approval, the case was ready for final processing. When fabricating immediate dentures, the author highly recommends using high-impact acrylic for the anterior portion in order to preserve the integrity of the prosthesis. In this case, GC Nature-Cryl Super Hi Impact acrylic (GC America, gcamerica.com) was chosen. This acrylic is available in 7 shades and is very impact resistant. To create the most esthetic denture possible, 2 shades of acrylic as well as a GC Gradia® gum (GC America) facing was used.6 The case was separated from the mounts and flasked in the traditional manner. The only modification was the use of laboratory putty on the facials of the teeth in order to allow for custom shading and the ease of deflasking (Figure 10). (Note: If only stone is used, the free monomer will etch through the separator and make removal of the stone challenging.) For this case, Nature-Cryl Light shade, which was defibered, was used in the areas of the free gingiva and the eminences.7 Light Reddish Pink was used as the base color. The case was trial packed 3 times on each arch with the use of the traditional press-packing technique and allowed to bench cure for 20 to 30 minutes. The dentures were cured for 9 hours at 165° F with a 30-minute boil afterward. When the curing was completed, the flasks were allowed to bench cool to room temperature and deflasked in a regular manner.
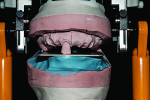
The deflasked dentures should remain on the master cast or be placed back onto it to assess whether they accidently moved during the deflasking process. The case was remounted and post-process equilibrated (Figure 11). This step is crucial in the fabrication of the prosthesis to evaluate any changes to occlusion that may take place during curing, especially when using the press-packing technique. After the case was equilibrated, it was removed from the master casts and polished (Figure 12). This was to ensure no stone or putty would remain anywhere on the case. The dentures still were not fully finished because a Gradia gum facing needed to be added in order to create a more natural appearance.
Using a composite on the surface of the prosthesis allows for a highly esthetic look and facilitates an increase of gingival contours if needed (especially in immediate dentures). The use of clinical photographs greatly helps in the selection of the proper colors to be selected for a specific patient. The case was roughly polished with silicone polishers, and gingival contours were reduced until just an outline was visible. The dentures were micro-etched with 50-micron aluminum oxide and cleaned with compressed air or cold-cure monomer. (Note: No steam should be used for fear that the introduction of moisture or oils would inhibit the bond between the composite and acrylic.)
The dentures were fully dried, and a composite primer was placed over the surface that would be accepting the Gradia gum composite. The prosthetic was placed in the GC Labolight LV-III (GC America) for 3 minutes. A mixture of gum modifiers was used in order to mimic the patient’s natural gingiva. GC Initial GM-35 was utilized on the free gingiva and eminences, GM-36 between the eminences and vestibular region, GM-34 in the vestibular region, and GM-32 and GM-31 in the attached gingival regions. Color intensifiers and mixes of the above modifiers were also used. The GC Steplight SL-1 (GC America) was used between the color applications to allow the composite to stay in place. Once all the colors were placed and the case was verified, the GC air barrier was placed and the final cure was performed using the GC Labolight for 3 minutes. The dentures were then steamed and polished with pumice. Instead of using a high-shine polish, Optiglaze (GC America) was used to seal the composite and bring a nice luster to the prosthesis.8
The prosthesis was sterilized and sent to the dental office for final delivery (Figure 13). Although in this particular case, the use of an alveoloplasty guide was not requested, many cases have it fabricated alongside the immediate completed removable prosthesis.
Once the remaining dentition was extracted, the dentures were immediately placed and adjusted. After the patient and dentist verified occlusion and esthetics, follow-up appointments for 24 hours, 1 week, and 2 weeks were scheduled (Figure 15).
Conclusion
Using the customized approach with the use of tinted acrylics and composite gingival overlay, technicians can create a prosthetic that has a more lifelike appearance and is generally well-accepted by the patient. This article demonstrates that immediate removable dental prosthetics can be highly esthetic and functional.
Acknowledgments
Clinical work was performed by Grant Matsuura, DDS.
References
1. Zarb GA, Hobkirk JA, Eckert SE, Jacob RF, eds. Prosthodontic Treatment for Edentulous Patients. 13th ed. St. Louis, MO: Mosby; 2013.
2. U.S. Naval Dental School. Navy training Course, Navpers 10685-C. Dental Technician, Prosthetic. 5th ed. Bethesda, MD: Bureau of Naval Personnel;1965.
3. Blakeslee RW, Renner RP, Shiu A. Dental Technology: Theory and Practice. St. Louis, MO: Mosby; 1980.
4. Merz Dental. TiF® - Total prosthetics in function. Merz Dental. https://www.en.merzdental.de/content/19.php. Accessed May 15, 2015.
5. Abe J, Kokubo K, Sato K. Mandibular Suction-Effective Denture and BPS: A Complete Guide. Tokyo, Japan: Quintessence Publishing Co. Ltd; 2012.
6. Shimizu H, Kawaguchi T, Yoshida K, Tsue F, Takahashi Y. Effect of surface preparation on the failure load of a highly filled composite resin bonded to a denture base resin. J Prosthodont. 2009;18(3):684–687.
7. Zaleske T. Nature-Cryl Tips & Tricks, Frequently Asked Questions, & Techniques with Tom Zaleske. Part 01. GC America Lab Marketing. https://www.youtube.com/watch?v=QJ3sSx8r8Uo. Accessed May 15, 2015.
8. Machida D, Kumagai T, Sakuma T, Akahane S. 0858 Effect of wear resistance improvement of Nano-filled resin coating. International Association for Dental Research. https://iadr.confex.com/iadr/2008Dallas/techprogram/abstract_101003.htm. Accessed May 15, 2015.