Use of Tuberosity Tissue Block for Tunneling Reconstruction of Class III Sockets With Simultaneous Implant Placement: A Case Report
Ramon Gomez-Meda, DDS; Jonathan Esquivel, DDS; and Markus B. Blatz, DMD, PhD
Abstract: Immediate implant placement in the anterior maxilla remains a complex procedure, particularly when the cortical bone plate of the socket is not intact and a gingival recession is present. The reconstruction of both hard and soft tissues increases the complexity of these clinical scenarios. This case report describes a novel, minimally invasive technique to reconstruct class III sockets with simultaneous implant placement. Four incisions are made with a scalpel blade to create, or "draw," a square outline instead of raising a flap at the tuberosity to harvest a hard- and soft-tissue block. In addition, a tunneling approach is described to graft the site while preserving the recipient area's vascularity. Harvesting a hard- and soft-tissue block from the tuberosity in a minimally invasive manner preserves the donor site and helps to reconstruct a class III alveolus in one single appointment, thereby reducing morbidity, costs, and treatment time.
To achieve optimal outcomes with an immediate implant clinicians must consider both surgical and prosthodontic parameters. These include hard- and soft-tissue quality and quantity, size and design of the dental implant, as well as adequate 3-dimensional position, primary stability, emergence profile, and final restoration esthetics.1
After tooth extraction, horizontal and vertical bone remodeling is unavoidable.2 Even though immediate implant placement in the anterior region is commonly done with predictability similar to delayed implant placement, it does not avert bone collapse after the periodontal ligament has been lost.1,3,4 Several protocols have been proposed to prevent this frequent complication.5-11 Endodontic failure, advanced periodontal disease, trauma, and root fracture are commonly linked to bone resorption and soft-tissue loss.7 In turn, the cortical bone plate may be heavily damaged, and immediate implant placement is contraindicated.12,13 Techniques have been described to reconstruct type II and type III sockets but are considerably aggressive or do not allow immediate implant provisionalization.7,14,15
This article presents a technique to reconstruct class III sockets with a predictable and minimally invasive approach that avoids raising flaps, thereby enabling the bone volume of the donor site to not be compromised while preserving the vascularization of the recipient site.
Case Report
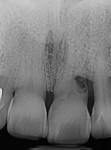
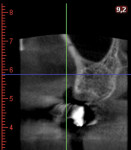
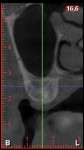
A healthy 71-year-old male patient presented with advanced periodontal disease and pain on the maxillary left central incisor. Upon radiographic analysis, an external root resorption was diagnosed, which caused gingival recession and a cortical bone defect on the facial aspect of the tooth (Figure 1 and Figure 2). Proximal bone volume and the distal interproximal papilla were compromised. Digital implant planning and surgical guide fabrication were done to facilitate precise implant placement (Figure 3).
After local anesthesia was administered, the tooth was extracted with a periotome. The epithelium of the alveolar sulcus was eliminated with a diamond bur, and the defect was measured with a periodontal probe (Figure 4). The implant site was prepared, and a 4.3 mm x 16 mm implant was placed (Figure 5). A digital impression was made, and a provisional crown was fabricated (Figure 6). A wide supraperiosteal tunnel was prepared on the buccal aspect of the pocket with a microblade past the mucogingival junction to allow the coronal repositioning of the soft tissues to cover the future graft.
The treatment plan called for harvesting a cortico-cancellous autogenous bone block with its connective tissue and epithelium from the tuberosity. Therefore, a segmental cone-beam computed tomography (CBCT) scan was taken to assess the dimensions of the tuberosity and the position of the sinus floor and to avoid oroantral communication. Soft-tissue thickness was evaluated with a periodontal probe, and a square outline was drawn on the right tuberosity with a 15C blade, reaching the bone. Incisions were made 2 mm away from the lateral margins of the tuberosity and 1 mm away from the distal surface of the last molar. Incisions were designed perpendicularly to the coronal aspect of the tuberosity and slightly angulated from the outer part to the inner side of the bone. The graft was then harvested with a bone chisel and mallet (Figure 7).
After deepening the chisel through the lateral and distal incisions, the last cut was made in the mesial incision, and the chisel was pushed mesially to detach the hard- and soft-tissue graft. The graft was then embedded in a saline solution and trimmed to be adapted to the receptor site. The soft tissue can also be de-epithelialized if necessary.
The bone harvested from the maxillary tuberosity was wedged into the gap of the buccal surface of the implant to cover the exposed implant threads. The harvested bone and soft-tissue block were inserted carefully into the tunnel, leaving the osseous portion beyond the limits of the bone defect (Figure 8). The graft was stabilized by fixating the connective tissue portion on the gingival flap with a combination of horizontal mattress and simple interrupted 6-0 monofilament sutures. Finally, the implant-supported provisional was used to help stabilize the graft and blood clot to obtain an esthetic outcome (Figure 9 and Figure 10).
The patient was prescribed amoxicillin 500 mg thrice daily for 7 days. Ibuprofen 600 mg was recommended only during the first day if necessary. He was instructed to rinse with 0.12% chlorhexidine gluconate twice a day. Sutures were removed 2 weeks later, and follow-ups were scheduled every 2 weeks during the first month.
After 4 months, the peri-implant soft tissues appeared healthy, and the probing depths ranged from 3 mm to 4 mm with no bleeding on probing. A digital impression was made, and the final implant-supported zirconia crown was delivered 2 weeks later. The bone around the implant head was radiographically stable at the 2-year follow-up, with only a slight sign of remodeling around the abutment connection (Figure 11 and Figure 12). The CBCT showed a buccal bone plate with 2 mm of thickness on the facial aspect of the implant, and no increase in gingival recession was noted (Figure 13).
Discussion
Proper case selection is paramount to successful results when placing immediate implants in the anterior maxilla.16,17 Bone and soft-tissue quality and quantity should be carefully analyzed. The present technique is indicated in class III sockets or class II sockets with a thin biotype, where bone reconstruction and soft-tissue thickening is needed. This technique increases the bone and soft-tissue volume as well as the band of keratinized tissue when the epithelium or connective tissue is left partially exposed. The connective tissue can also be grafted under the papilla in patients with periodontal disease where the proximal gingival volume is compromised. The soft tissue protects the bone grafted and helps to seal the socket. At the same time, the provisional restoration stabilizes and protects the graft. Consequently, the practitioner can obtain predictable and successful long-term results, reducing the treatment time, morbidity, and costs for the patient.
After tooth extraction, horizontal and vertical bone resorption of the facial cortical plate occurs, which may lead to recession and an incomplete papilla due to the lack of support of the facial mucosa.2,3 Thus, implant treatment goals must include reconstructing these lost anatomic structures. At least 1.5 mm of bone and 2 mm of soft-tissue thickness are recommended to avoid a future gingival recession on the implant-supported crown's facial aspect.18,19 Therefore, the implant selected should allow a 3-mm gap between its body and the cortical plate.20
In 2014, da Rosa and coworkers published a technique to reconstruct the hard and soft tissues simultaneously with a triple graft from the tuberosity. However, unless using the technique described in this case report, the graft was harvested after raising a flap.14 The external cortical bone plate of the tuberosity was then harvested along with a piece of connective tissue graft, compromising the future volume of the tuberosity as the external bone plate was extracted. Also, a small flap was raised on the recipient site's facial aspect to allow graft placement. Conversely, the presented technique avoids damaging the tuberosity's bone walls, preserving its volume. As a result, an auto-regenerating defect is created, which, as demonstrated in this case, heals spontaneously (Figure 14 through Figure 16). At the recipient site, a tunnel approach is used to avoid any vertical or angulated releasing incisions, thereby better preserving the vascularization of the area.
Zufia and coworkers published another approach to grafting periodontal sockets. The four-layer graft made of cortico-cancellous bone, epithelium, and connective tissue was used to cover the implant completely, reconstructing the bone and soft-tissue volume vertically and horizontally.15 At the same time, the keratinized band was improved. The technique, however, does not allow for the immediate loading of the implant, is more technique sensitive, and requires more appointments than the technique described herein.
The present technique achieves functional and esthetic results with high predictability. It is less complex than the ones described previously due to the straightforward graft design, in which the graft can be trimmed after harvesting to fit the facial defect of the socket to be treated, fully or partially de-epithelializing the graft if necessary.
The stabilization of a thick graft tissue in a localized buccal wall defect is the most challenging part of the treatment of damaged sockets. The main drawback is that a tuberosity with sufficient bone volume is needed so as to leave at least 2 mm of bone underneath the sinus floor to avoid oroantral communication. Also, access to the donor site may be difficult, especially in patients with a small mouth opening.
Conclusion
A minimally invasive technique was presented for the reconstruction of class III sockets with simultaneous implant placement. It utilized four incisions to create a square outline rather than raising a flap at the tuberosity to harvest a hard- and soft-tissue block. It also used a tunneling technique. This technique is aimed at preserving the donor site and facilitating reconstruction of a class III alveolus with reduced morbidity, costs, and treatment time.
About the Authors
Ramon Gomez-Meda, DDS
Adjunct Assistant Professor, Louisiana State University Health Science Center (LSUHSC) School of Dentistry, New Orleans, Louisiana; Private Practice, Ponferrada, Spain
Jonathan Esquivel, DDS
Associate Professor, Department of Prosthodontics, Louisiana State University Health Science Center (LSUHSC) School of Dentistry, New Orleans, Louisiana
Markus B. Blatz, DMD, PhD
Professor of Restorative Dentistry, Chair, Department of Preventive and Restorative Sciences, and Assistant Dean, Digital Innovation and Professional Development, University of Pennsylvania School of Dental Medicine, Philadelphia, Pennsylvania
References
1. Del Fabbro M, Ceresoli V, Taschieri S, et al. Immediate loading of postextraction implants in the esthetic area: systematic review of the literature. Clin Implant Dent Relat Res. 2015;17(1):52-70.
2. Araújo MG, Lindhe J. Dimensional ridge alterations following tooth extraction. An experimental study in the dog. J Clin Periodontol. 2005;32(2):212-218.
3. Botticelli D, Berglundh T, Lindhe J. Hard-tissue alterations following immediate implant placement in extraction sites. J Clin Periodontol. 2004;31(10):820-828.
4. Cosyn J, Eghbali A, Hermans A, et al. A 5-year prospective study on single immediate implants in the aesthetic zone. J Clin Periodontol. 2016;43(8):702-709.
5. Tsuda H, Rungcharassaeng K, Kan JY, et al. Peri-implant tissue response following connective tissue and bone grafting in conjunction with immediate single-tooth replacement in the esthetic zone: a case series. Int J Oral Maxillofac Implants. 2011;26(2):427-436.
6. Cabello G, Rioboo M, Fábrega JG. Immediate placement and restoration of implants in the aesthetic zone with a trimodal approach: soft tissue alterations and its relation to gingival biotype. Clin Oral Implants Res. 2013;24(10):1094-1100.
7. da Rosa JC, Rosa AC, da Rosa DM, Zardo CM. Immediate dentoalveolar restoration of compromised sockets: a novel technique. Eur J Esthet Dent. 2013;8(3):432-443.
8. Sarnachiaro GO, Chu SJ, Sarnachiaro E, et al. Immediate implant placement into extraction sockets with labial plate dehiscence defects: a clinical case series. Clin Implant Dent Relat Res. 2016;18(4):821-829.
9. Assaf JH, Assaf DD, Antoniazzi RP, et al. Correction of buccal dehiscence during immediate implant placement using the flapless technique: a tomographic evaluation. J Periodontol. 2017;88(2):173-180.
10. Sanz M, Lindhe J, Alcaraz J, et al. The effect of placing a bone replacement graft in the gap at immediately placed implants: a randomized clinical trial. Clin Oral Implants Res. 2017;28(8):902-910.
11. Khoury F, Doliveux R. The bone core technique for the augmentation of limited bony defects: five-year prospective study with a new minimally invasive technique. Int J Periodontics Restorative Dent. 2018;38(2):199-207.
12. Buser D, Martin W, Belser UC. Optimizing esthetics for implant restorations in the anterior maxilla: anatomic and surgical considerations. Int J Oral Maxillofac Implants. 2004;19 suppl:43-61.
13. Bäumer D, Zuhr O, Rebele S, et al. The socket-shield technique: first histological, clinical, and volumetrical observations after separation of the buccal tooth segment - a pilot study. Clin Implant Dent Relat Res. 2015;17(1):71-82.
14. da Rosa JC, Rosa AC, Fadanelli MA, Sotto-Maior BS. Immediate implant placement, reconstruction of compromised sockets, and repair of gingival recession with a triple graft from the maxillary tuberosity: a variation of the immediate dentoalveolar restoration technique. J Prosthet Dent. 2014;112(4):717-722.
15. Zufía J, Blasi G, Gómez-Meda R, Blasi A. The four-layer graft technique, a hard and soft tissue graft from the tuberosity in one piece. J Esthet Restor Dent. 2019;31(4):304-310.
16. Elian N, Cho SC, Froum S, et al. A simplified socket classification and repair technique. Pract Proced Aesthet Dent. 2007;19(2):99-104.
17. Kan JY, Roe P, Rungcharassaeng K, et al. Classification of sagittal root position in relation to the anterior maxillary osseous housing for immediate implant placement: a cone beam computed tomography study. Int J Oral Maxillofac Implants. 2011;26(4):873-876.
18. Spray JR, Black CG, Morris HF, Ochi S. The influence of bone thickness on facial marginal bone response: stage 1 placement through stage 2 uncovering. Ann Periodontol. 2000;5(1):119-128.
19. Thoma DS, Mühlemann S, Jung RE. Critical soft-tissue dimensions with dental implants and treatment concepts. Periodontol 2000. 2014;66(1):106-118.
20. Rosa AC, da Rosa JC, Dias Pereira LA, et al. Guidelines for selecting the implant diameter during immediate implant placement of a fresh extraction socket: a case series. Int J Periodontics Restorative Dent. 2016;36(3):401-407.